The report, published in 2004, gained support from the late Sir Richard Doll, the eminent epidemiologist who co-discovered the link between smoking and lung cancer. He had completed a clinical trial which found that people who took vitamin D supplements may live longer – and had he lived had wanted to do another. It has taken eight years to get that clinical trial started with Professor Julian Peto of the London School of Hygiene and Tropical Medicine. Called VIDAL, the trial is looking at benefits of supplementation and for any increase in life expectancy in over 65s.
Highlighting the benefits of vitamin D has led to at least some degree of change in official attitudes. We are now advised to spend some time in the sun at midday, while vitamin D supplements are advised for breastfed (but not bottlefed) babies from the first month of life.
My belief is that we could go much further – that vitamin D, given freely to all women in pregnancy, could be used to curb or prevent some major diseases including multiple sclerosis, diabetes, schizophrenia, asthma and several cancers; and that it might also be used to treat established disease, at least in early stages.
One crucial piece in the jigsaw has come from the study of birthdays. Links between birthdays and future life events have long been the territory of clairvoyants and mediums; and when evidence first emerged about a decade ago that people born at the end of winter were more likely to get multiple sclerosis and those born in autumn less so, many scientists found it hardly credible.
“It looked as if we were interested in star signs and futurology,” said George Ebers, emeritus professor in the Department of Department of Clinical Neurology at the Wellcome Trust Centre for Human Genetics, University of Oxford, whose career has never deviated from scientific correctness. “But now we know that MS is associated with end of winter births, when shortage of sunshine is demonstrable and vitamin D levels are lowest. This suggests, in line with other observations, that vitamin D protects against the disease.”
THE POWER OF THE SUMMER SUN
Summer sun is at its maximum in June and July but vitamin D, generated in the skin by sunlight, takes two or three months to get into the general circulation. So we reach our maximum level of vitamin D in about September. Babies born in October or November have the best chance of a relatively high level of vitamin D during their final months in the womb. And this, the birthday evidence suggests, can protect them from MS, while the risk is higher for babies born at the end of winter.
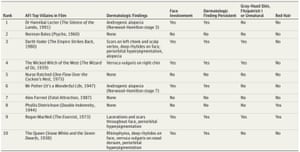
This seasonal pattern in the risk of MS has now been found in eight different countries including Australia, winning over previously sceptical scientists. Less well known is the link between end of winter birthdays and an increased risk of several other diseases. Studies of thousands of birthdays in Europe, Canada and Australia over some 30 years have found that people born at this time are also at greater risk of type 1 diabetes, coeliac disease (gluten intolerance), schizophrenia and autism.
People with winter birthdays are at greater risk of type 1 diabetes
For a long time experts did not know what to make of this data, since these diseases had no obvious links. But now more conditions are being added to this list by the Oxford team. Writing in the peer-reviewed journal, BMC Medicine, in July 2012, Professor Ebers, working with Dr Sreeram Ramagopalan, has shown that the risk of rheumatoid arthritis, a digestive disease called ulcerative colitis and a distressing condition called systemic lupus erythematosus follows the same pattern of seasonal births. These are all autoimmune diseases, which occur when the body is attacked by its own immune system. Diabetes type 1 is also an autoimmune disease and in the case of coeliac disease the immune reaction is to wheat in the bowel. To date, at least 18 autoimmune diseases have been linked to low vitamin D levels – more than enough to demonstrate a pattern.
”These immune-mediated diseases are one of the most common disease groups in modern economies today, affecting some 10% of the world population. Vitamin D deficiency is the most obvious risk factor” says Dr Ramagopalan. To test this theory Dr Ramagopalan has examined blood taken from the umbilical cords of 50 healthy babies born in November and 50 born in May when, after winter, levels of vitamin D are low. The May babies had a far higher frequency of newly generated white blood cells called T cells which are normally programmed to react against infection by an outside agent and to tolerate the body’s own tissues.
However certain types of T cells react against the body tissues and they may cause autoimmune disease later on if they persist. These unwanted T cells are normally removed from the body in the first year of life by a clever arrangement – they are deleted in the thymus gland, a process that requires vitamin D. So a low vitamin D
level leaves the baby at risk. Dr Ramagopalan has explained his findings in detail in the open access, peer-reviewed PLOS Genetics, 2009, in which he writes: “The prevalence of diseases, such as multiple sclerosis, type 1 diabetes, inflammatory bowel disease, and rheumatoid arthritis correlate positively with latitude and reduced ultraviolet radiation exposure which is the primary determinant of vitamin D levels.”
The scientific jigsaw is now making more sense, but some pieces still do not seem to fit. Why should schizophrenia, a mental health condition, be linked to season of birth? In fact the birthday evidence on schizophrenia has provided a vital scientific clue to a disease which has puzzled doctors for over 100 years. Researchers now recognise that schizophrenia also has features of an autoimmune disease in which the body attacks its own tissues.
Schizophrenia and MS are both diseases of the nervous system. In MS myelin nerve sheaths deep in the nervous system are attacked by an immune reaction. If this can happen in MS, surely it is not so strange that schizophrenia may be explained similarly by an immune attack on crucial areas of the brain.
Dr John McGrath, international expert in schizophrenia based at the University of Queensland, Australia, says the evidence suggests that sun exposure in pregnancy and early life protects against schizophrenia and “raises the tantalising prospect that optimising vitamin D status during pregnancy may lead to the primary prevention of the disease”.
“Being born in the country where there is more opportunity for sun exposure is associated with a lower risk of schizophrenia – while moving subsequently to an urban area where more time is spent indoors does not seem to increase the risk,” he points out.
Could lack of vitamin D in pregnancy also explain autism? The latest evidence suggests that a low vitamin D level in the mother’s body during pregnancy may induce her immune system to make antibodies which can damage the baby’s brain, as well as causing certain genes to malfunction. Last month, Rhonda Patrick and Bruce Ames from the Children’s Hospital Oakland Research Institute, in California, published research findings that these genes normally make the chemical serotonin.
Too little of this neurotransmitter is associated with abnormal social behaviour while too much in the digestive tract causes sensitivity to foods which may explain some autistic children’s difficult eating habits.
Patrick and Ames, both well-respected scientists in the field of autism, suggest: “Supplementation with vitamin D and tryptophan [which is made into serotonin in the brain] is a practical and affordable solution to help autism and possibly ameliorate some of the symptoms of the disorder.”
But the vitamin D jigsaw puzzle is not finished yet. Some 15 or more different cancers have been consistently associated with low vitamin D levels in a way that accords with established criteria, according to epidemiologist Dr William B Grant, from the non-profit organisation the Sunlight Nutrition and Health Research Center in California. In his paper published in 2009, the link is most clearly seen in breast and bowel cancer. Insufficient vitamin D leads to loss of control of several genes which regulate proliferation of cancer cells and inhibit the cell cycle.
In fact there are more than 900 genes that Vitamin D is now known to switch on and off – and in doing so alters our vulnerability to disease. The large number of genes involved explains how so many quite different diseases can be caused by insufficient sunshine. In this way sunshine exposure directly alters the action of genes which may actually be passed on in their altered state – a newly understood process known as epigenetics. So it is possible to see how some diseases may emerge for the first time in one generation and be passed on to the next.
There is understandable opposition to these theories from some in the medical establishment. In an editorial published last December,the journal The Lancet argued that failure of “gold standard” clinical trials of vitamin D to treat disease in adults disproves the possibility that insufficient vitamin D is a causal factor.
In my view, this ignores a wealth of experimental and observational evidence associating low vitamin D levels with higher risk of certain diseases. Also, vitamin D given in adulthood cannot necessarily be expected to cure a condition that has arisen through lack of vitamin D in early life. This is an error in scientific reasoning which I call the The Lancet’s “gold standard fallacy”.
INDOOR LIFESTYLES BLAMED
At the same time researchers are finding links between vitamin D and chronic disease, the world is facing an epidemic of these same conditions, caused by our indoor lifestyles. Even in the height of summer people in cities often have sub-optimal levels of vitamin D, and so babies born at any time of year may develop these diseases. It’s well recognised that multiple sclerosis has become increasingly common in the UK over the last century. Today, in cloudy Orkney, off the north of Scotland, one in 150 women suffer from MS, believed to be the highest prevalence in the world.
Less well known is that a generation ago the disease was much less common in southern than in northern Europe. But MS has increased rapidly in the Mediterranean over recent years, reflecting the increased movement of people away from rural subsistence farming to town and a life in urban apartments. In the Greek island of Crete MS has increased almost four fold over the last generation.
Between 1989 and 2006, the incidence of MS in Iran increased more than eight fold
One striking example of the rise in MS is in Iran where, after the Islamic revolution in 1979, women were compelled by law to wear the veil outdoors together with clothing covering most of the body. Between 1989 and 2006, the incidence of MS in Iran increased more than eight fold, from an incidence of about one case in 100,000 to nearly one in 10,000 in the city of Isfahan.
“The Islamic revolution can potentially explain the observed increase in MS incidence in Iran in just over 30 years,” said Dr Ramagopalan. “Veiled women have lower vitamin D levels compared to unveiled women, giving an increased risk of low vitamin D in pregnancy which can account for the increase in MS.”
There have been similar increases in other autoimmune diseases, some rare or even unknown a century ago. Type 1 diabetes has seen an annual 4 per cent increase across Europe in a generation, with larger increases in the under-fives and the number of cases in this age group expected to double between 2005 and 2020. Crohn’s disease, a life threatening inflammation of the bowel, has since the 1930s become increasingly common in most developed countries.
Between 1965 and 1997 the incidence of schizophrenia doubled in London’s Camberwell. Much, but not all, of the increase is attributed to second generation dark-skinned immigrants who have a five times greater risk of the disease than their parents or people with white skin. Dark skin blocks absorption of weak northern sunlight, preventing vitamin D synthesis.
Autism was also rarity a generation ago. Between 1988 and 1995 the incidence in UK children increased some five fold, according to a nationwide survey by a 1000 GPs; arguably such a large rise cannot all be explained as improvements or changes in diagnosis of the condition, which is generally held to be difficult to miss. A similar increase occurred in the United States in the 1990s.
Over the last generation there has also been a global increase in asthma. Tests on frozen blood show that the epidemic is not caused by changes in diagnosis. Allergic reactions to mixed pollens, animal dander and house dust mites have increased by 4.5 per cent per decade in the UK during last quarter of the 20th epidemic has been followed closely by a rapid increase in food allergy. In extreme cases allergy can cause anaphylactic shock which has increased in England by 50 per cent between 2001 and 2005.
Professionals dealing with overflowing clinics are talking about a ‘double tsunami’ – a giant wave of asthma followed by a second wave of food allergy, suggesting that they are two parts of a continuing epidemic. Two distinguished professors, Augusto Litonjua and Scot Weiss, from Harvard University School of Medicine calculate that some 300 million people worldwide now suffer from asthma and blame social changes: “…as populations grow more prosperous and more westernised”, they say, “more time is spent indoors and there is less exposure to sunlight, leading to vitamin D deficiency, subsequently resulting in more asthma and allergy.”
Why has the wave of food allergy followed the wave of asthma rather than occurring simultaneously: and why are second generation immigrants more at risk of diseases such as schizophrenia or Crohn’s than their first generation parents? The new science of epigenetics explains how the environment can influence genes which are then passed on in an altered state, in apparent contradiction of classical genetics.
Women who are severely vitamin D deficient may pass on de-activated genes, which make their children more vulnerable to disease. Multiple sclerosis, Type 1 diabetes, Crohn’s, schizophrenia, autism, asthma and food allergy have all been increasing in the same overlapping time frame and all have links to low vitamin D and low sunshine exposure. A further 11 autoimmune diseases have been linked to serious vitamin D deficiency in an Oxford study published in BMC Medicine in 2013. This makes at least 18 autoimmune diseases clearly linked to low vitamin D levels – more than enough to demonstrate a pattern.
PREVENTION IS CRUCIAL
Although The Lancet may insist otherwise, some clinical trials have shown that people with MS, asthma or Crohn’s may do better or have fewer relapses when they take vitamin D, if disease is not too advanced. For example, MS begins with optic neuritis, a temporary form of blindness, in 20 per cent of cases. Doctors at Isfahan University, Iran, have shown in a clinical trial that giving vitamin D (about 7,000 IUs per day) at this early stage can reduce risk of a relapse in blindness by 68 per cent and lower the incidence of lesions and “black holes” in the brain. They are hopeful that vitamin D may delay the usual conversion of optic neuritis to subsequent MS. Symptoms of Crohns’ disease can be reduced dramatically by 5,000 IUs per day of vitamin D according to a clinical trial at the Center for Molecular Immunology, University of Pennsylvania. Another study at Massachusetts General Hospital, described in the journal Inflammatory Bowel Disease, 2013, shows that risk of surgery is reduced in Crohns’ patients who took a vitamin D supplement that increased their blood level to normal.
While the Lancet remains trapped in its “gold standard” fallacy, doctors working with these autoimmune diseases, previously sceptical, are now privately hopeful that vitamin D will prove to be a useful addition to treatment. But increasing vitamin D later in life cannot always restore what has been lost when vitamin levels are low: for example, in the case of diabetes type 1, an enterovirus may attack the islet cells in the pancreas that make insulin, wiping them out. This is why prevention is so crucial: the link between high vitamin D levels in pregnancy and a reduction in diabetes risk was shown as long ago as 2001.
The UK has arguably one of the unhealthiest climates in the world
BRITAIN’S CLOUDY SKIES ARE BAD NEWS
THE UK has least sunshine of almost any advanced economy; our cloudy weather is arguably one of the unhealthiest climates in the world. And even when the sun shines we spend too much time indoors, detained by our computers and TVs. Fear of sunlight has been spread by misguided advice from cancer charities urging people to “seek the shade” rather than enjoy the sun safely and often. Extensive use of suncreams since the 1970s, has reduced exposure to UVB, the part of sunlight which generates vitamin D. The Chief Medical Officer, Dame Sally Davies, has said she is “profoundly ashamed” at the return of rickets in the UK. But the increase in rickets is small compared with the pandemic of immune system disease, the cost of which can be calculated in billions. MS costs the UK £3 billion a year, type 1 diabetes £9 billion, and schizophrenia £12 billion
IN 1942, when Britain was besieged by German submarines, the government was eager to maintain the nation’s health by providing all children with cod liver oil, the best natural source of vitamin D. Since then successive governments have pursued a false economy and restricted free supplies of vitamin D supplements to a small percentage of pregnant and breastfeeding women and under-fives who are on state benefits.
I believe a great advance could be made by returning to heroic wartime thinking, providing all pregnant women and babies with free vitamin D supplements. I would argue that an intensive programme reaching 80-90 per cent of people, as modern vaccinations do, would greatly reduce and might even virtually eradicate MS, type 1 diabetes and several other autoimmune diseases.
Even lesser measures could at least halt or slow the pandemic. At little cost, the government could encourage voluntary fortification of foods such as milk and bread with vitamin D and give better advice on benefits of sunshine and how to enjoy the sun safely. Failure to act soon will be a cause for profound national shame.
Oliver Gillie is an award-winning writer and scientist. His report Sunlight Robbery: Health benefits of Sunlight are Denied by current Public Health policy in the UK can be downloaded from http://www.healthresearchforum.org.uk/
Vitamin D - could it quit "modern" conditions?