Harvey’s reaction to his dementia is not what you might expect. “I’m so happy,” he says. “I wouldn’t reverse it for anything.”
Harvey has a relatively rare dementia called posterior cortical atrophy or PCA, a variant of Alzheimer’s disease. Inasmuch as he has difficulty remembering things and can’t do basic arithmetic, his condition conforms to the stereotype of dementia. But PCA particularly affects spatial awareness: it can lead to disorientation, visual illusions, and problems with making your movements coincide with your perception of space. Harvey has trouble with vests; another person with PCA recounts how, aiming to sit in an empty seat, he found himself instead in his vicar’s lap. But for Harvey, who is 78, these are just inconveniences in a wonderful life. He has never, he says, felt so full of love for his wife, Diana, who confirms that his expressions of affection are much more frequent now than before his PCA developed.
Harvey and Diana might be considered the lucky ones. Plenty of people with PCA, and their families and carers, have grimmer stories to tell. But there are many cases that challenge the widespread perception of dementia as a condition to be dreaded. The stereotype of an elderly loved one sitting blankly in a care home, unable to speak or recognise relatives, is not all there is to it. And changing this public perception of dementia is one of the prime objectives of a £1m, two-year project called Created Out of Mind .
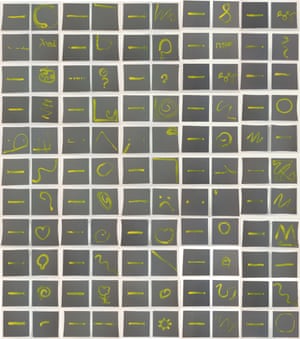
Music for Life 360 uses machine learning to analyse interactions between musicians and people with dementia
Supported by the Wellcome Trust and housed in its Hub space at the top of the Wellcome Collection on Euston Road in London, Created Out of Mind is the brainchild of Sebastian Crutch, a neuropsychologist in the Dementia Research Centre of University College London. As well as challenging stereotypes about what it means to live with dementia, the project aims to develop better tools for assessing the value of using arts with people who have these conditions. All too often, such efforts are perceived as “giving them something to do”, or perhaps as utilitarian therapies for sustaining cognitive skills. But if the real personal enrichment of the arts often comes “in the moment”, why should it be any different for people with dementia? And such activities can reveal a creativity obscured by impairment of an individual’s resources for regular communication.
When Crutch asked me to join the research team, I gladly accepted the opportunity to learn more about a condition that will affect most of us in our lifetime – if not as a patient then as a carer or relative. My own experience of having to gently assure my grandmother that she was still living in the house she had occupied since before I was born, and not in some unfamiliar care home where all her knick-knacks had been arranged in a simulacrum of her house, is representative of experiences most of us have had, or will have.
Alzheimer’s disease is the most familiar form of dementia, but it accounts for only about one case in three, and itself has many variants with specific symptoms. There is a galaxy of other dementias, generally diagnosed from their cognitive symptoms and perhaps brain scanning. Other neurodegenerative conditions such as Parkinson’s disease can also progress to dementia. And not all forms of dementia happen in old age – some can appear in people still in their 30s.
Neither are they all about loss of memory. It may be precisely because we are used to the experience of forgetting things like names or where we left our keys that we read the appearance of dementia as forgetfulness. But sometimes the mental disruptions that look superficially like memory loss are actually operating in a more puzzling way. Asked if she can recognise photos of famous faces – Tony Blair, Bill Clinton, Terry Wogan – one person with PCA in a video Crutch shows me can name none of them. But it’s not so much that she doesn’t recognise the face; she struggles to see it as a face. “That’s the face there, isn’t it?” she asks hesitantly as she looks at Wogan.
It’s not a lack of recognition – the patient could say perfectly well who Blair or Wogan is. Her situation seems to be akin to that experience of seeing an image or an object, perhaps when we’re tired, and being momentarily unable to decode its content: is that a face, or the folds in an item of clothing? We can see clearly enough but can’t parse the shapes and shadows. “For a person with PCA, much of the world is of that ilk,” says Crutch.
What’s lost here are not facts, but ways to interpret the world. Some forms of dementia can affect how we label concepts, or our ability to retrieve those linguistic tags. Crutch shows me clinical videos of two people with primary progressive aphasia (PPA), which affects such aspects of semantic processing. One man speaks haltingly, slurring his words, sometimes getting the syllables wrong. The sentences are perfectly coherent but are produced with great difficulty. There’s no impediment to the way his mouth moves, but he’s struggling to connect words to the appropriate sounds. This man, says Crutch, carried a card he could show to explain why he was articulating in this way – otherwise people might think he was drunk.

The other PPA patient has degeneration a little farther back in the part of the brain where language is processed (the temporal lobes), impairing not word production but access to its semantic content. He is almost hyperfluent, articulating his words accurately and rapidly. The trouble is, he has lost the labels. He explains that he has been tying back his roses, but can’t describe them generically as plants, nor mention concepts like stem and thorn. Instead, with unselfconscious improvisation, he explains with finger gestures that they are things that branch and then branch again, and have those things on them that might puncture holes in your hands. “I can’t remember what you call them now, but we’ve got a thing that comes up, and they’re like that, and they’ve got all little bits on it…”
In such cases, less common words vanish sooner than ones used more often. Testing patients with animal recognition, “iguana” disappears before “dog”. Eventually this leads to extreme category errors: a less familiar image of, say, a gorilla might be interpreted, tentatively, as a car, not because that’s what it “looks like” to the patient but because he has so few categories of any sort to call upon in making an interpretation. This might tell us something about how we encode concepts mentally: perhaps we simply do more of that for familiar ones, so that we still retain some reference points when others are lost.
These are confusions in the brain’s ability to represent the world semantically. By contrast, in conditions like PCA, lesions in a different part of the brain can disrupt the “how?” or “where?” – the sense of space. One patient, asked to grasp the doctor’s right hand, does so easily. But he can’t make out where the left hand is at all, even though it is held just as clearly in front of him. After some guidance, he spots it – but asked then to take hold of it, he misses entirely and grasps the doctor’s shoulder. These spatial tasks are processed by both sides of the brain, each side dealing with the opposite region of space. So the lesions in this patient are probably concentrated on the left-hand side.
It’s hard for us to imagine this – it’s not at all like having only one eye working. “Everyone thinks vision means eyesight – they don’t connect vision problems with dementia,” says Crutch. But most people with Alzheimer’s will experience visual impairment at some stage, he says.
Harvey, a former electronics engineer who played drums and piano in a jazz band for much of his life, has his own experience of such spatial distortions. He was playing the piano when suddenly the keyboard seemed to have risen by four inches. Another time the keys seemed to disappear. As it is, he can no longer remember what the notes are called, nor can he decode written music (“all those lines!”). But like many jazz musicians, he plays primarily by ear, and still practises for several hours a day. In that still poorly understood miracle of the musical mind, he finds his fingers can keep going when his conscious mind cannot, constructing complex jazz chords that surprise him.
The visual illusions of PCA can be deeply disconcerting. Helen, a woman caring for her mother now in an advanced stage of the condition, tells me that her mother would furiously accuse her husband and other relatives of playing tricks on her when the coffee jar suddenly “reappeared” from where it had vanished a moment ago. This kind of irritable response, while wearing for carers, is a natural strategy for rationalising the confusion. Objects don’t disappear without a “reason”! Helen says her mother went through umpteen pairs of glasses, apparently a typical experience in the early stages of PCA.

At the beginning, the visual distortions can come and go, often prompting frustration or disbelief from others. Helen explains that her mother would occasionally lose the ability to navigate drinking from a cup – but at other times it was fine. “Even her best friends didn’t believe her,” she says.
Care home workers can’t possibly know all the nuances of dementias, and are generally used to working with people showing the gradual, predictable decline in abilities that comes with Alzheimer’s. It’s understandable, then, that they might not appreciate that because a patient like Helen’s mother has just taken a sip of tea, she might not be able to do so in five minutes’ time. It’s not hard to see how this could lead to suspicions of “playing up”, especially when patients are themselves made grumpy by the difficulties.
Perhaps most disconcerting of all are visual hallucinations of the sort that can be produced by the relatively common condition called “dementia with Lewy bodies” (DLB), which sometimes occurs alongside Alzheimer’s. One person in Seb’s videos talks clearly and calmly about finding his house full of people dashing about.
“I came home one night, and all of a sudden there were people in the room,” he says. “There must have been at least a dozen, running and screaming everywhere. When you see that, you panic yourself – you don’t expect anyone in your own living room. One was dressed like Coco the clown. I thought I was dreaming.”
Seeing people is quite common with DLB, but other hallucinations can be more surreal. One person diagnosed with the condition told Crutch that when he looked at table edges and door frames, he saw them bending. But his rational brain knew that this couldn’t be true.
There’s the problem: it’s not so much that you’re seeing things that aren’t there, but that our brains, still retaining the power of reasoning, have to deal with impossible information. “How do you hold that tension between the two things without driving yourself mad?” Crutch asks. And who can we trust, if we can’t rely on our own senses? Even the man who saw Coco the clown in his living room admitted scepticism about being told he was just hallucinating. How can we go on and on dismissing what we’ve seen if it doesn’t seem to fit with what we know ought to be so?
Seen this way, says Crutch, responses from some dementia patients that might be interpreted as aggressive, paranoid or obnoxious might in some respects be perfectly normal reactions to an unfaithful mind – all the more so when the condition has developed beyond the point of a patient’s conscious ability to rationalise away their hallucinations. If your handbag is “not where you left it”, isn’t it reasonable to conclude that the care home staff have stolen it?
A particularly distressing form of the confusion that DLB can induce is called Capgras syndrome. Here the patient recognizes a carer or family member but loses the ability to connect that individual to the one they remember. They become convinced that he or she has been replaced by an impostor.
One woman described her husband’s experience of this condition. “He said, who are you and what are your duties here? So I said, Well, I’m Betty. And he said, Yes, but you’re not the Betty I know. I said, There’s only me. That’s when he started walking up and down the stairs, going in and out of the rooms, wouldn’t sleep.”
It seems such a bizarre belief that the invitation is to imagine the person has totally “lost their marbles”. But on the contrary, says Crutch, the “impostor” interpretation is also a reasonable deduction. “If it doesn’t feel like the person you know, then you’re not being irrational, you’re trying to use the rationality available to you to explain the experience.”
Dementia is mostly, and rightly, associated with deficits of one kind or another in mental abilities. But the mind is extraordinarily inventive about circumventing difficulties or improvising with what it has to hand, and it’s not so surprising then that these neural gymnastics might introduce new aspects of personality, new interests and capacities. These might be puzzling or bewildering to people who see a loved one change, but as Harvey attests, the results need not be solely negative. Someone might develop a hitherto unseen passion for opera. They might take up painting with almost manic energy. Or they might discover new facets of their creativity.
In the case of British artist William Utermohlen, who was diagnosed with Alzheimer’s in 1995, painting enabled him to create an extraordinarily expressive testament to his disintegrating sense of self. Utermohlen’s self-portraits, produced over the following five years, have been widely hailed as offering an insight into the condition. The final portrait, painted in 2000, seven years before his death, is a pencil-drawn head with two black holes for eyes, suggestive of a soft toy long neglected in the dust of a playroom.
But what remains intact in all these images is a sense of artistic integrity – their increasing abstraction sacrifices nothing of the power. Crutch visited Utermohlen in his flat in late 1999, when he still retained some ability to communicate. He was able to indicate how one striking self-portrait at his desk under a skylight, with one hand clinging to the corner, reflected his sense of desperately trying to hang on and avoid being swept out of the open window. “I suspect that the painting was more eloquent than anything he could have said at the time he painted it,” says Crutch.
Some see this as no different from the artist’s usual practice of conscious self-expression, albeit with diminishing resources. But Crutch is convinced that not everything in such art might be there by intention; the works might also testify to the nature of the condition. When Utermohlen was in their research centre at UCL, they asked him to draw a man. Far from the stick figure most of us would have produced, Utermohlen produced a beautiful sketch full of charm and wit. But there was something amiss. He knew it, but couldn’t figure out what it was.
To Crutch, and to most of us, it couldn’t be more plain: both of the figure’s arms were coming out of the same shoulder socket. This was a classic example of the spatial confusion of PCA. “I absolutely deny that this was his artistic intent,” says Crutch. “His tools had just been blunted.”
As well as seeking to change public perceptions of dementia, Created Out of Mind hopes to explore the role of the arts in these conditions. In projects such as Music for Life 360, which uses machine learning to analyse interactions between musicians and people with dementia, and a study of psychological and hormonal responses of a choral group, researchers will be seeking new ways to measure the effects of engaging in artistic activities.
Very often, initiatives such as this are seen solely therapeutically: as “good for the patient”. There’s no doubt this can be true, but as Utermohlen showed, they have far greater potential. Because arts may involve different parts of the brain – different communicative pathways – from the faculties of daily interaction such as talking, they might help to keep channels open. It’s very common for patients who might have become nonverbal to respond to music, perhaps even to sing.
The temptation is to respond that “At least she remembers something!” But there could be more to it than that. As conditions like PPA show, loss of language use doesn’t necessarily imply loss of understanding or desire to interact verbally. In fact, the extreme deterioration of that ability can produce some incredibly poignant testimonies to the inventiveness and determination of people to communicate. One man with PPA was, in the late stages of his condition, left with only two words: “Millionaire” and “Bub”. But, says Crutch, he would manage with just those severely depleted resources to express feelings and responses with the tone of his voice.
So arts aren’t just a “way of keeping them occupied”, but may become avenues for releasing genuine creativity. It’s easy to assume with people rendered mute by dementia that their understanding and inner life has gone just as silent. “You hear time and time again from carers who use music with patients that suddenly there’s a reconnection,” says Crutch. They often say not that this has transformed the patient but that it confirms that the awareness they always thought was there really is there.
Susanna Howard, founder of the charity Living Words, works with people with dementia to produce poetry (see panel). The remarkable, often moving results show the form’s capacity to express the person’s experience:
We lost a lot of nice things, all kinds –
They go away. A little bit I got here and then
All of a sudden there was nothing I could tell you.
Could not put two together. I had a lovely story
But it took my – you know, when I found out
I couldn’t talk mouth ways, like now,
I can’t think.
These points of connection are reminders for us, the healthy ones, that the person with dementia, who doesn’t know who we are any more and can’t talk and doesn’t even seem to see us, is still a person.
“Because we focus so much on the verbal, there’s an underlying lack of clarity about what these people actually experience when they can’t tell us any more,” says Crutch.
Lacking their direct testimony, we’re apt to make assumptions about it – which might obscure the person now for what we imagine them to have once been. This engagement with the present is precisely what the arts can offer, says Julian West, an oboist and researcher at the Royal Academy of Music. West has for years made music with people affected by dementia, for example in the Music for Life project at London’s Wigmore Hall.
“A few years ago I was working with a woman who was a Holocaust survivor,” he tells me. “She had very little capacity for verbal communication, and there was a lot of anxiety surrounding her, with carers worrying about how her dementia might ‘unleash’ memories of her experiences. The ‘in the moment’ experience, however, was that she looked at everyone with bright, animated eyes, and was very engaged with the music-making. At a pause, she made eye contact with me and very playfully sang ‘cuckoo’. I and the other two musicians were able to then improvise a piece with her based on her cuckoo motif, which she continued to sing. It was an expression of her playfulness and energy, and let us relate to her as she wanted to be rather than through our worries about her.”
West continues: “The focus of the work I am involved with is not at all about ‘helping people to remember’. I sometimes wonder whether the perceived need for people with dementia to remember things is more important for family, friends and carers. The idea that someone can retain value and identity independent of memory and capacity is outside many people’s thinking, and so the loss of memory is very frightening for them.
“The arts are a powerful vehicle for helping everybody to understand more of the complexity and diversity of people’s experiences,” says Crutch,”and to adjust ourselves to better maintain our social contact. Again and again we come across people who say: what really helped us to understand this person was connecting through music, or sharing in a response to a picture, or a carer seeing someone who can still create something. It can still be about who they are, not just who they were.”
Words unlocked: dementia and poetry
Making poetry with people with dementia takes time, explains Susanna Howard, artistic director of the project Living Words. She typically spends several months in a care home, generally with people with advanced dementia – beyond the point of reminiscence. “We don’t ask any questions,” she says. “We sit in silence in the shared experience with the participant, and as words come we write them down and read them back to the person.
“All words matter. It can be the smallest, seemingly insignificant words a person uses that have the most meaning for them, and we write every word down without trying to ‘make sense’ of them. ‘I don’t know’ or ‘Nothing’ says a lot about how that person is feeling.”

One person she worked with recently kept repeating under her breath, “I am the woman no one is watching.”
Then the editing begins. “We slowly start stripping away, reading their words back and seeing whether they resonate with the person. We only remove – we never add or jiggle words and meaning around. The intention is that the pieces are being written for that person, for them to feel validated. Often you can be reading a person’s words to them and they say ‘Yes, that’s just how I feel.’” The titles of these pieces are usually the first response that the person has on hearing their words read to them: Want People To Know What It’s Like, Can’t Think, I’m An Okay, All You Got.
This is deep work, Howard says. “We have the luxury of time to sit with people one-to-one. And it’s about equality of relationship within the creative process – the person is not ‘having art done to them’ but is actively engaged in meaningful shared experience.”
There can be direct therapeutic benefits. “This is like medicine to me,” said one care home resident. It offers social interaction and can encourage better relationships with caregivers, and allows people to feel heard and validated.
The results, however, reach beyond the personal. Like the best poetry, what they offer is a direct, stripped-down truth: a communication where, perhaps, none seemed any longer possible.
Speaking
This place is mad, it is
I think, think it’s good
To get out, I’m speaking
Look at round there
They’re wanting me now
A mad one, near
Don’t say much
It will come
The lost word
Forgetting but not gone: dementia and the arts
Hiç yorum yok:
Yorum Gönder